Abdominal Aortic Aneurysm (AAA)
AAAs have a modern approach to their management through non-surgical and surgical treatments. When surgery is necessary, intervention through bilateral groin regions allows for deployment of stent grafts with minimal recovery time.
How did I develop an Abdominal Aortic Aneurysm (AAA)?
There are many factors that can put you at risk of developing an AAA. Some may be hereditary and others may be related to your lifestyle.
Common risk factors for abdominal aortic aneurysm (AAA) development include:
Hypertension (high blood pressure).
Smoking.
Age greater than 65.
Male gender.
Inherited connective tissue disorders: Marfan syndrome, Ehlers-Danlos syndrome and collagen vascular diseases.
Chronic obstructive pulmonary disease (COPD).
Coronary artery disease (CAD) or heart disease.
Those with a first degree relative with an abdominal aortic aneurysm are at a greater risk.
Infection or inflammation.
Trauma.
How are Abdominal Aortic Aneurysms (AAA) diagnosed?
There may be no symptoms until the AAA has enlarged significantly, is leaking or has ruptured. In this instance, symptoms that are reported would include abdominal, lower back, groin or chest pain.
A physician may note a pulsating mass under the skin of your abdomen, or hear abnormal blood flow sounds when listening with a stethoscope.
Tests that can confirm diagnosis:
Abdominal ultrasound.
Computed tomography (CT) scan.
Magnetic resonance imaging (MRI).
What are my treatment options for an Abdominal Aortic Aneurysm (AAA)?
If your AAA has been discovered early and is still small (less than 5 centimeters), surgery may not yet be necessary. In this case, your vascular surgeon will closely monitor the growth of your aneurysm every 6-12 months by obtaining computed tomography (CT) scans.
Additionally, it is important to quit smoking and control your risk factors, such as keeping your blood pressure under control with medication.
Once your aneurysm has reached 5 centimeters, the risk of rupture is much higher, and surgery is recommended. Your vascular surgeon will decide what the best options are for you at that time and discuss complications and risks. There are two choices for treatment:
Traditional Open Repair of AAA
A large surgical incision is made into your abdomen to directly visualize your AAA. The aneurysm is opened, and a cylinder-like tube known as a graft is sewn inside to repair it. The weakened area of the aorta is relined with a sleeve of material to strengthen it and prevent rupture of the aneurysm. Hospital stay with this procedure is about 5 days, with full recovery at 6 weeks.
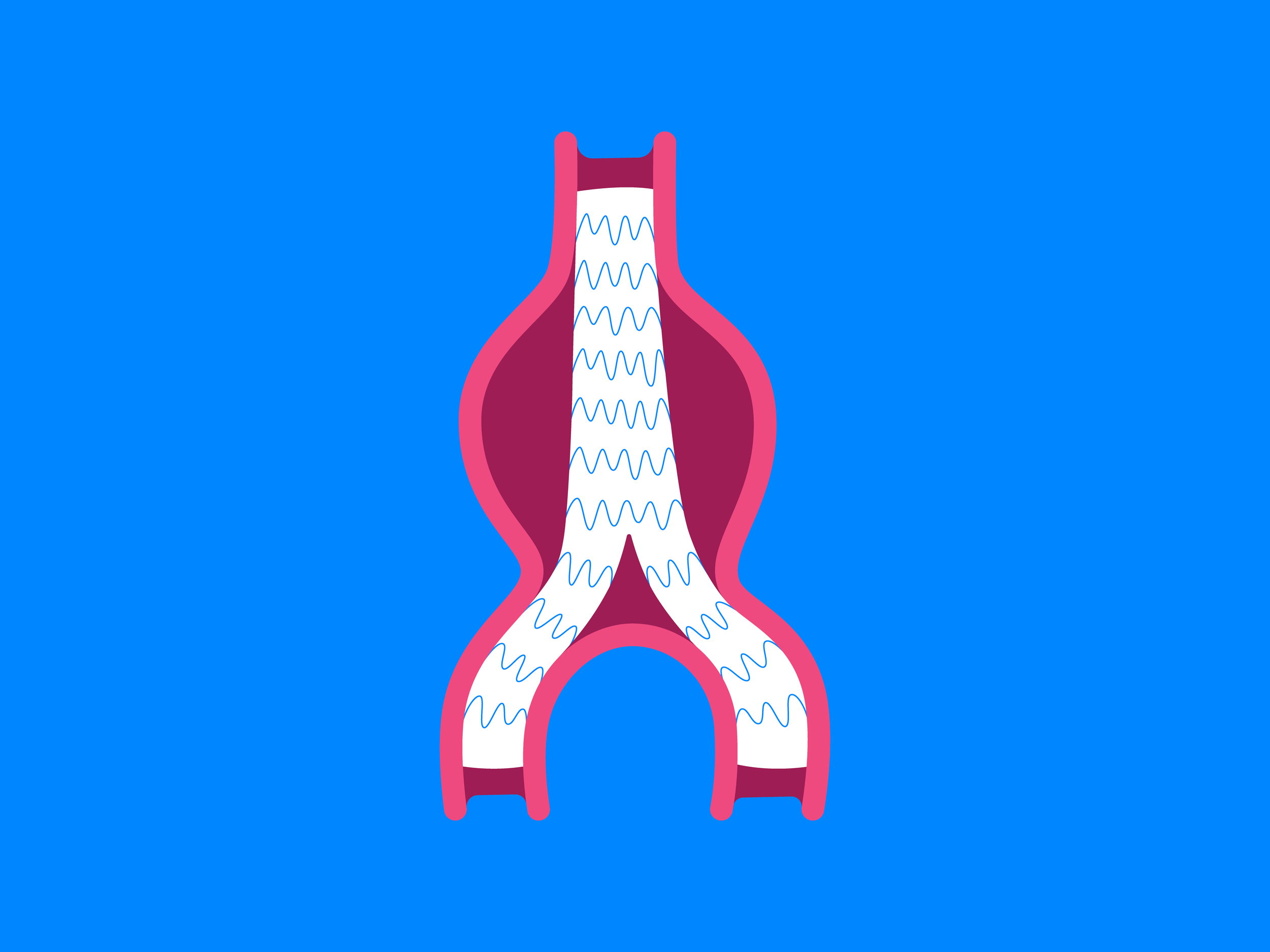
Endovascular Repair of AAA
A less invasive approach than traditional surgery, this repair involves only a small incision in the groin. Endovascular means that the procedure uses long thin tubes inside your body called catheters. Under guidance of an x-ray, a small catheter is placed through the groin incision and used to pass a cylinder-like tube called a graft up into the aneurysm. This graft is placed so that the ends fit neatly into the non-diseased portion of the artery at the opposite ends of the aneurysm. This is relining the weakened area of the aorta with a strong sleeve of material, thus preventing rupture of the aneurysm. Hospital stay for this procedure is about 1 day, with full recovery in about 1 week.
Abdominal Aortic Aneurysm (AAA) Procedure
Where is the AAA Procedure performed and who performs it?
The AAA procedure is performed in the hospital surgical suite by a vascular surgeon.
How do I find out if I am a candidate for the AAA Procedure?
To find out if you are a candidate for the AAA procedure, please request an appointment by calling Vascular Health Clinics at (989) 254-6427.